Start Your Support Journey
Is your family looking for support as you navigate a diagnosis of epilepsy or seizure disorder? Are you looking to connect with other families who have a child with epilepsy? Complete our intake form so that we can serve you better and provide the resources and activities that would be most helpful to your family.
About Epilepsy
What is Epilepsy?
Epilepsy is a neurological condition which affects the nervous system. Epilepsy is usually diagnosed after a person has had at least two unprovoked seizures that were more than twenty-four hours apart. It is important to note that not every seizure is due to epilepsy. If a person who is NOT KNOWN to have epilepsy has a seizure, it is a medical emergency, and you should call 911. Epilepsy affects every person differently depending on age, types of seizures, response to treatment and whether or not the person has other health issues, etc. Epilepsy affects people from all communities, many of whom do not have any family history of seizures. While the exact causes of epilepsy are varied and not entirely known, epilepsy and seizures typically result from abnormal signals from neurons (a type of brain cell) in the brain. It can be genetic, meaning it is the result of mutations in a person’s genes, or it can be acquired through events such as physical injury or infection. In up to 70% of epilepsy cases worldwide, the cause is idiopathic, which means unknown. In 30% of cases, epilepsy is acquired through certain illnesses or events. Some underlying causes of acquired epilepsy include:- Brain structure abnormalities
- Head trauma
- Infectious disease
- Stroke
- Tumors
Demographics
Epilepsy is considered one of the most prevalent neurological disorders globally.
- 1 in 26 Americans will develop epilepsy in their lifetime.
- An estimated 3.4 million Americans and 65 million people worldwide currently live with epilepsy.
- Each year more than 150,000 people are diagnosed with epilepsy.
- Per the CDC, 456,000 children in the United States 17 and younger have active epilepsy.
- Epilepsy is the fourth most common neurological disorder.
- Epilepsy affects more people than multiple sclerosis, cerebral palsy, Parkinson’s disease, and ALS combined.
What Is a Seizure?
A seizure is a burst of uncontrolled signals between brain cells. Seizures alter one or more of the following:
- Movement
- Sensation
- Behavior
- Awareness
Seizures generally last a few seconds to a few minutes and can range from brief lapses in attention to bodily convulsions.
There are many different types of seizures and they can present differently based on multiple factors, including where the seizure originates in the brain. People with epilepsy can have one type of seizure or several types of seizures.
Seizures are usually classified into three main groups: Focal Onset, Generalized Onset, or Unknown Onset.
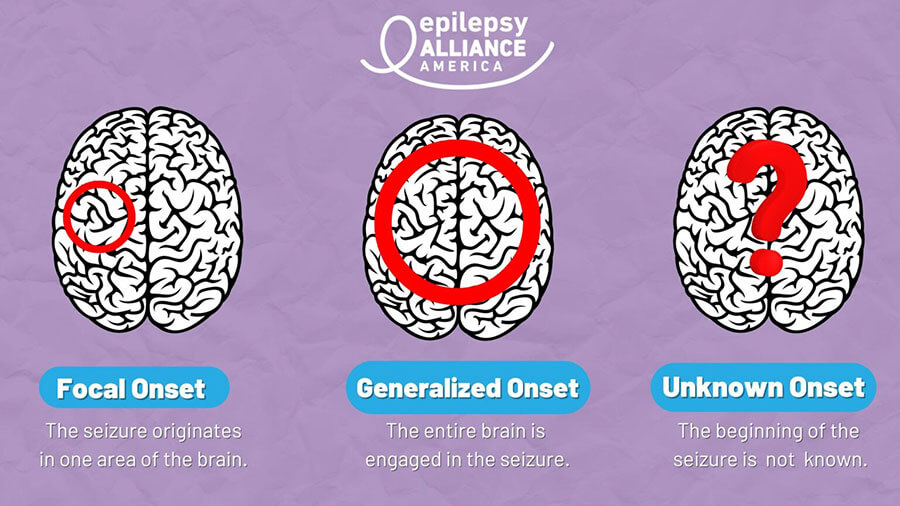
Focal Onset
In focal onset seizures, the seizure originates in one specific part of the brain. Note that this seizure activity can spread to involve more of the brain and transition into a tonic-clonic seizure.
Focal Onset Seizures can also be divided into different types based on the effect on the person’s awareness level.
- Focal Onset with Impaired Awareness
- Focal Onset with Awareness Maintained
These seizures can present with motor symptoms (falling, jerking, chewing) or non-motor symptoms (changes to cognition, emotion, sensation).
Focal Onset Seizures with Impaired Awareness (older term: complex partial) will change a person’s awareness. The seizure may start with a blank stare, followed by repeated movements (called automatisms). These seizures are sometimes confused with drunkenness, drug use, mental illness, disorderly conduct, or acting out. A person will not be able to respond to verbal instructions during this type of seizure and afterward, the person may seem confused and not remember what happened. These seizures typically last 1-2 minutes.
Focal Onset Seizures with Awareness Maintained (older term: simple partial) – With this type of seizure, full awareness is maintained, and the person can display rhythmic movements, such as isolated twitching of arms, legs, or face. Typical symptoms of this type of seizure are sensory feelings such as tingling, weakness, and visual distortions or psychic symptoms such as feelings of déjà vu, hallucinations, or unexplained anxiety. These seizures may be confused with acting out, mystical experiences, or psychosomatic illness. There may also be isolated twitching of arms, legs, or face. This type of seizure usually lasts less than one minute.
Generalized Onset Seizures
Generalized onset seizures involve both sides of the brain and include four primary types:
- Tonic-Clonic
- Absence
- Myoclonic
- Atonic
Tonic-Clonic Seizures (older term: grand mal) are the most recognized type of seizure. These seizures involve stiffening and jerking convulsions of the body and limbs. Other typical symptoms are loss of consciousness and collapsing and can also cause difficulty breathing and loss of bladder or bowel control. This type of seizure usually lasts one to three minutes. After a tonic-clonic seizure, the individual may be tired, disoriented, or have a headache. Call an ambulance if the seizure lasts longer than 5 minutes, if it is the person’s first seizure, or if the person is pregnant or has diabetes. Never restrain someone having a tonic-clonic seizure and never place any items in their mouth.
Absence Seizures are often mistaken for daydreaming or lack of attention. These seizures typically last a few seconds and can happen many times throughout the day. These seizures cause a brief lapse of awareness that causes a person to have a blank stare. During an absence seizure, a person will not be able to respond and will not have an awareness of what’s going on around them. After, they will typically become conscious right away. Epilepsy Alliance America is proud to have supported this white paper on childhood absence epilepsy, which also led to this informative webinar.
The last two types of Generalized Onset Seizures are atonic Seizures and myoclonic seizures.
Atonic Seizures cause a sudden loss of muscle tone that usually leads to a fall and loss of consciousness. Head and facial injuries are common with these types of seizures.
Myoclonic Seizures are often confused with clumsiness or poor coordination. They are characterized by sudden, brief muscle jerks that usually last a few seconds, with the person maintaining consciousness.

Seizure Triggers
Certain events or situations may increase the likelihood of a seizure occurring in people with epilepsy; these are called seizure triggers. Some common triggers include:
- Use of alcohol or drugs
- Flashing lights
- Stress
- Not getting enough sleep
- Certain types of foods, caffeine
- Changes in blood sugar
- Common cold, flu, or other illness
- Menstruation
- Missed medication
Triggers vary from person to person, and an individual may have multiple triggers.
Diagnosis & Treatment
While the diagnostic process will vary for each person, the major steps in the process should include:- Detailed medical history – may include questions regarding the mother’s pregnancy and delivery, any relatives with epilepsy, and whether the person had a high fever, serious head injury and/or periods of staring, inattention or breath-holding.
- Detailed account of seizure – the person(s) who was present at the time of the individual’s seizure is advised to communicate what (s)he saw with the doctor.
- Physical examination – the exam may include assessment of cardiac, neurological and mental status.
- Blood test – a blood test(s) may be ordered to identify potential causes and/or identify other significant illness(es).
- CAT (Computerized Axial Tomography) or CT Scan – may be ordered to determine whether a seizure has been caused by an acute neurological lesion or illness.
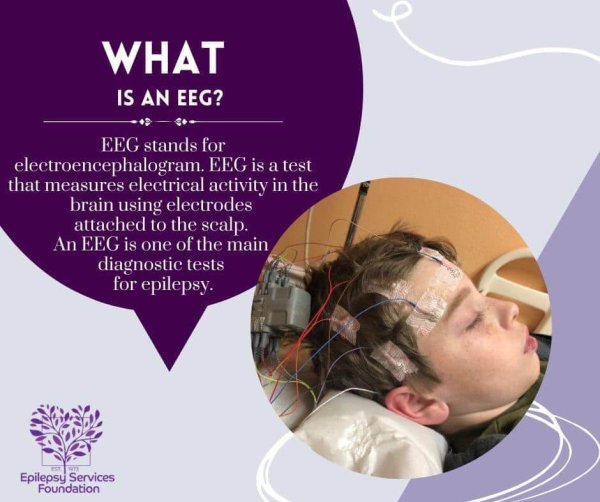
- EEG (Electroencephalogram) – shows the brain wave activity that can be used to assess the risk of seizure recurrence, and it may also help determine seizure type.
- MRI (Magnetic Resonance Imaging) – a preferred brain picture when evaluating persons with new onset seizures or seizures that may have started in a particular area of the brain.
Seizure Treatments
Anti-Seizure Medications
The most common first treatment is medication. There are currently more than 30 medications available to treat seizures. The doctor will choose the best one depending on the seizure type and syndrome, as well as possible side effects or other medications a person might be taking. Most types of medications are taken by mouth in the form of tablets, capsules, sprinkles, or syrup.
Different people react in different ways to anti-seizure medications. One drug may effectively control one person’s seizures, while that same drug may not work at all for another person. A person may need to try several different medications before finding a treatment that works to control seizures without negative side effects. Do not feel discouraged; this is typical for many people. Often, doctors will prescribe more than one kind of seizure medication because together they may work better than any of the medications taken alone. It is important to stay optimistic and patient during this time.
Taking medication at the prescribed time every day is an important part of the treatment. The medicine taken every day replaces what has been used by the body, keeping the medication level at the correct therapeutic level in the bloodstream. Skipping a dose, taking fewer pills than prescribed, or not filling a prescription on time can cause the medication level to be too low in the blood, increasing the risk of a seizure.
Ketogenic Diet
Prescribed by a doctor, the ketogenic diet is an extremely strict diet that helps to stop or control seizures for some children. It should be treated like a serious medication and must be closely supervised by a dietician, physician, and the child’s family. The diet is carefully tailored for the individual child, and the types and amounts of food the child eats must be strictly regulated.
The diet, which is very high in fat and very low in proteins and carbohydrates, produces a change in the child’s body chemistry called “ketosis.” Ketosis has an anti-seizure effect in about 2 out of every 3 children who try the diet. Not all doctors agree that this diet is good for children who have seizures.
The ketogenic diet is prescribed for children for a limited amount of time. After remaining on the diet for a while, doctors and the dietician will want to slowly taper off the diet and reintroduce regular food. If seizures return, the diet may be reinstituted. Studies are being conducted now to determine if the ketogenic diet may be an effective form of treatment for adults.
Implantable Devices
Vagal Nerve Stimulation (VNS) Device
With VNS, a surgeon implants a small device with a wire and battery (about 2 inches in diameter) in the upper left chest. The device sends regular bursts of electricity at a regular interval along the left vagus nerve in the neck, via some electrodes that doctors will wrap around the nerve. This regular flow of electricity along this particular nerve has an anti-seizure effect in some patients who try it as a form of treatment.
If a person has a VNS and experiences an aura, or senses that they are about to have a seizure, they can swipe a specially designed magnet over the implant, which will trigger it to send some electricity along the vagus nerve to prevent the seizure from happening. Family, friends, and caregivers can also swipe the magnet over the implant during a seizure in the hopes of reducing the length or severity of the seizure.
Some of the newer VNS devices can detect changes in heart rate that are associated with seizures, and will automatically send an extra signal/stimulation. The VNS is used in addition to anti-seizure medications. The newest VNS device is approved for children as young as four.
Responsive Neurostimulation (RNS) Device
This device, currently only approved for adults 18 years and older, is used in addition to anti-seizure medications. With an RNS device, a surgeon places the neurostimulator under the scalp in the skull, with one or two wires that connect to the part of the brain where seizures start. The device records brain activity and senses when a seizure is about to start. It then sends pulses of electricity to stop or lessen the seizure.
Surgery
Brain surgery can be an effective treatment for epilepsy, but it isn’t right for everyone. Generally, doctors will consider many factors first and will recommend surgery only as a last resort. The doctor may suggest surgery when:
- A person has tried multiple anti-seizure medications without success
- The seizures always start in one part of the brain
- The seizures are in a part of the brain that can be safely removed without damaging the ability to speak, see, or remember
- The seizures are caused by another problem in the brain, such as a tumor
Surgery for epilepsy will most likely be performed at special medical centers, rather than local hospitals. In addition to operations that remove part of a patient’s brain, other types of surgeries can be performed to interrupt the spread of electrical disturbances in a person’s brain.
Patients are often awake during brain surgery since the brain does not feel any pain. Having the patient stay awake helps the surgeons make sure that important parts of the brain are not being damaged during the operation.
After brain surgery for epilepsy, a patient will most likely still have to take anti-seizure medications for a year or two. If no seizures occur during this time, the doctor may slowly wean the person off of the medication. Some people are able to live seizure- and medication-free from this point on; however, many people still need to take their anti-seizure medication(s), and some have seizures that continue.
____
Infantile Spasms
For more information on infantile spasms, click on the button below.What is PNES and how is it diagnosed?
Psychogenic nonepileptic seizures (PNES) is a disorder characterized by events that mimic epileptic seizures but are not caused by abnormal brain activity. Events related to PNES have an underlying psychological cause. Other terms for PNES are psychogenic seizures or pseudoseizures. The term pseudoseizure is discouraged as it can unintentionally lead others to believe the seizures are not real. PNES is a serious diagnosis and should be treated as such.
The exact cause of PNES is unknown. It is a subtype of a conversion disorder. For people with PNES, their bodies convert an emotional response into a physical response. It is important to remember that the person does not have control over this response.
As it can be difficult for PNES to be distinguished from epileptic seizures, patients will often see a neurologist, and the doctor will begin by taking a thorough medical history. Tests such as a routine electroencephalogram (EEG) or magnetic resonance imaging (MRI) may also be ordered.
The Nonepileptic Seizure Task Force of the International League Against Epilepsy indicates that Video-EEG (vEEG) is the gold standard for diagnosis of PNES. During a vEEG, the patient’s brain waves are monitored by the EEG and any events are recorded on video. The video will allow doctors to review any behaviors or sounds that occur during the event. If a person is experiencing multiple seizure types, each type should be captured by vEEG.
However, vEEG is not always available, and a doctor with experience in diagnosing seizure disorders may be able to diagnose PNES without vEEG. Psychogenic seizures have different characteristics than epileptic seizures, and an experienced doctor may be able to recognize these differences, particularly if a seizure is witnessed by the doctor or if someone else is able to record a seizure on video.
Frequently Asked Questions about PNES
What is the treatment for PNES?
Antiepileptic drugs will not treat PNES and may even increase events. Once diagnosed, patients with PNES should seek psychiatric and psychological health care for treatment.
Cognitive Behavioral Therapy (CBT) is a psychological treatment that has been shown to be effective in managing many mental health disorders, including PNES. CBT can help a person to identify unhelpful thinking and behaviors and teach helpful coping skills, which may result in symptom relief. Research has been shown that CBT may help control psychogenic seizures, however, other psychological therapies, such as individual therapy or group therapy, may be beneficial as well.
Can you have both epilepsy and PNES?
Yes, a person can have both conditions during his/her life or these conditions may even occur at the same time. This is why each seizure type needs to be documented.
Can people with PNES drive?
Dr. Robert Trobliger authored a paper that was published in Epilepsy and Behavior on patients diagnosed with PNES and resumption of driving.
Additional resources regarding PNES / Functional Seizures can be found here.
Primary content provided by Epilepsy Alliance Louisiana and Epilepsy Alliance America
National
Transportation Options
In addition to using a car, bus, train or bicycle, there are other transportation options for persons with epilepsy in the West Central Florida area.
Uber has a rideshare app. There is a low cost: about $5-7 to ride almost 3 miles. Ask you doctor if they offer UberHealth.
Lyft has a rideshare app. The cost: $0.90/mile plus a service fee of $1.90. Minimum fare is $3.50. Ask your doctor if they offer Lyft Concierge.
TBARTA is a carpooling service. This ride sharing company is only for persons employed and who need transportation to and from work. A person receives a personalized computer match-list of persons who live and work near the person needing this service. Cost is determined by the company. You register on-line: www.tbarta.com/en/carpooling/commuter/carpool You can also call TBARTA for information at 1.800.998.7433.
Carpool World is another carpooling service. It is similar to TBARTA except that the cost is decided between the persons and not the company. You register on-line: https://www.carpoolworld.com
Mercy Medical Angels provides assistance in the air with commercial airline tickets and volunteer pilots, and on the ground with gas cards, bus and train tickets.
Transitioning to Adult Care
If you have a teen or pre-teen who will soon be transitioning from pediatric to adult care, you may have many questions on how to make this transition as smooth as possible. Click the link below to access some helpful resources!
Service Dogs & Devices
Epilepsy Service Dogs and Training
- Canines 4 Hope – Palm City, Florida 1.855.885.6262 Provides dog and dog training Cost: $16,000 – $24,000. Family must cover costs or fundraise the money. It takes 6 months to a year for a dog to be placed.
- Magnolia Paws for Compassion – Helping to raise awareness of the benefits animals provide for those coping with illness.
- Canine Assistants– Located in Georgia. Provides dogs for free. Waiting time may be 1-5 years. Canine Assistants educates and places seizure response dogs with individuals with epilepsy and seizure disorders. Following general education, seizure response dogs are taught to remain next to a recipient during the course of a seizure, summon help in a controlled environment, or retrieve a phone prior to a seizure when indicated by the recipient. Some dogs may even develop the ability to predict and react in advance to an oncoming seizure once they are placed with their recipient.
- 4 Paws for Ability – 4 Paws for Ability is a non-profit organization that breeds, raises, trains, and places service dogs with children and veterans who have disabilities. Founded by Karen Shirk in 1998, the organization has grown from a one-bedroom apartment to a purpose-built campus in Xenia, OH with more than sixty staff members and thousands of volunteers.
- Kids and Canines – Dorothy Thomas Center – Tampa FL. 33618 Process: Call 813-986-2118. This is an assistance dog training program, gives middle school teens a new “leash” on life. Each student is paired with a dog in order to train the dog to be a helpmate to an individual with disabilities, or a child with autism. Cost: Unknown
Seizure Detecting Devices
Empatica – The Embrace wristwatch was developed by Empatica, Inc. The watch is able to detect seizures in persons with epilepsy and can alert a smartphone app or a “companion” watch worn by a parent, spouse, roommate, or anyone who will be close to the wearer when seizures are likely to occur. The watch also measures stress levels which can trigger seizures.- Cost: Approximately $199.
- www.empatica.com
- Cost: go to www.smart-monitor.com
- For more information, visit SAMi’s website at www.samialert.com.
- SAMi pricing: $399


